General microbiology - viruses, bacteria, fungi >>>> How bacteria resist antibiotic therapy
How bacteria resist antibiotic therapy.
For mankind, the mechanism of confronting various harmful microorganisms from year to year is becoming more and more complex, since the pace of development of methods for combating pathogens begins to lag behind the ability of pathogenic microorganisms to resist the destructive action of various biochemical compounds.
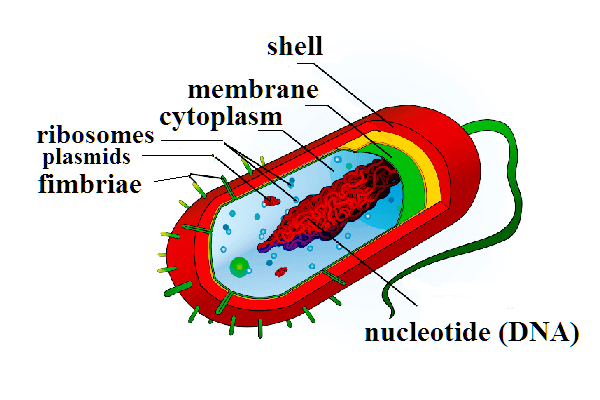
Let us analyze the mechanism of action of drugs on pathogens and the methods of resistance available in microorganisms using bacteria as an example. To understand the mechanism of action of antibacterial drugs, you need to remember the structure of the bacterial cell:
- The cell wall of the bacterium gives it its shape and holds the internal cellular elements.
- The cytoplasmic membrane of a bacterial cell adheres from the inside to the cell wall, separating it from the cytoplasm.
- The cytoplasm fills the cell from the inside and contains a mixture of different organic elements: ribosomes and RNA, nucleoid (in which DNA is located) and others.
All antibiotic therapy drugs are accordingly divided into groups that differ in the mechanism of action on certain cellular structures - targets (cellular and cytoplasmic membranes, processes of synthesis and metabolism):
- Cell wall synthesis inhibitors (Penicillins, Monobactams, Cephalosporins, Carbapenems, Glycopeptides, Bacitracin, Cycloserine) destructively act on the formation of the cell wall, and its strength is lost.
- The protective functions of the cytoplasmic membrane are affected by inhibitors of the functions of the cytoplasmic membrane (Polymyxins).
- Folic acid metabolism is disturbed by antimetabolites (Sulfonamides, Trimethoprim).
- Protein synthesis inhibitors of ribosomes (Tetracyclines, Aminoglycosides, Macrolides, Chloramphenicol, Lincomycin) inhibit protein synthesis, and they do not act on human ribosomes (another structure).
- Nucleic acid synthesis inhibitors (Quinolones, Rifampicin) disrupt DNA and RNA synthesis (chain formation).
Bacteria also have a significant arsenal at their disposal to preserve their colonies:
- Targets are modified, that is, mutations of bacterial cellular structures occur in such a way that the mechanisms of interaction of chemical compounds with targets are disrupted, up to the complete loss of these contacts. For example, bacteria E. Coli or Pseudomonas aeruginosa, rearranging the cell membrane from modified proteins (nonspecific proteins), thereby reduce the sensitivity to antibiotic therapy
- Protect targets, that is, bacteria are capable of synthesizing special proteins that bind to the target, modify it and cancel the effect of antibacterial drugs, for example, tetracyclines and quinolones.
- They inactivate, that is, by means of enzymes, they modify or destroy antibiotics (for example, they attach phosphates or acetylene to their chemical structures, which breaks the bonds with the ribosomes of the bacteria). Bacteria received this property from nature to protect their body from antibiotics produced by them. But what is interesting is that these mechanisms cannot inactivate synthetic antibacterial drugs, but only natural antibiotics (for example, Penicillins or antibiotics obtained from the Streptomyces bacteria).
- They have special transport systems in the cell membrane for the removal of antibacterial drugs from the cell, while simultaneously forming acquired resistance.
- They reduce the permeability of the bacterial membrane (this method is typical for gram-negative bacteria) by disrupting the permeability of the porin channels through which antibacterial substances enter the bacterial cell.
All of the listed mechanisms of protection of bacteria from antibacterial drugs can be attributed to the mechanisms of resistance. There are a number of ways in which bacteria acquire mechanisms of resistance in the course of their vital activity. Previously, science believed that in the process of evolutionary improvement, bacterial offspring acquired gene constructs, in which resistance was fixed as a factor that improves the structure of bacteria as a species that is a useful property of the organism, passed down from generation to generation. But now research in this area confirms the theory that bacteria can transmit the property of resistance not only to generations, but also to share it among themselves. This method of transferring resistance to antibacterial substances from one bacterium to another is called horizontal, as opposed to the transfer of developed resistance by reproduction (vertical). Horizontal transfer by means of genetic elements is a phenomenal ability that is discovered exclusively in bacteria, it has not been found in plant and animal cells.
It is believed that bacteria obtained some defense mechanisms against antibacterial drugs precisely by means of horizontal transfer: genes encoding the work of transport systems for the elimination of compounds chemically harmful to bacteria; proteins that encode the work of enzymes to change the formula of antibacterial substances; proteins that protect ribosomes. For example, this is how resistance to antibiotic therapy arose in enterobacteriaceae (E. coli, Escherichia, Salmonella).
Bacteria in their structure have extrachromosomal mobile genetic elements: transposons and plasmids.
Plasmids involved in the transfer of resistance properties (more precisely, R-plasmids or R-factors) are ring-shaped DNA molecules of bacteria that exist independently of the genomic chromosomes of the bacteria and reproduce autonomously. They are passed from a carrier bacterium to another bacterium when they come into contact by conjugation (unidirectional transfer of genetic material).
Transposons are fragments of bacterial DNA capable of independent movement. These mobile pieces of DNA are responsible for transferring resistance between plasmids, chromosomes, and phages.
An interesting way of transferring resistance using phages (or transduction ), which, when multiplying in a bacterial cell, are incorporated into its genome, capture some of the genetic elements that generate resistance, and transfer them. In this case, the bacteriophage does not multiply, but is in a prophage state . The spread of resistance to antibacterial therapy by phage transduction among gram-positive bacteria (streptococci, staphylococci) and gram-negative bacteria E. coli was noticed.
Bacteria acquired the ability to resist (resistance) in the process of evolutionary struggle with other micro- and macroorganisms for existence and, it seems, are not going to concede to humans the right to life in their common habitat.

Read

Read