Digestive system >>>> Dyskinesia of the esophagus, causes and treatment
Dyskinesia of the esophagus, causes and treatment.
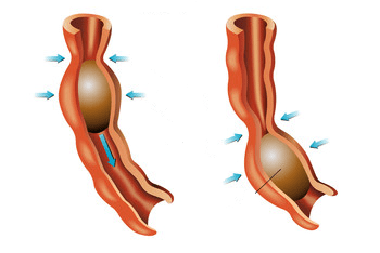
Dyskinesia of the esophagus is a disease associated with impaired motor (motor) function of the esophagus and its patency, leading to an abnormally slow movement of the food bolus from the pharynx to the stomach. At the same time, there are no changes in the structure of the tissues of the esophagus.
Etiology and pathogenesis
Dyskinesia of the esophagus can develop as an independent disease (primary dyskinesia). And also the functioning of the esophagus can be influenced by other concomitant diseases of the esophagus and digestive organs or diseases of other organs (secondary dyskinesia). Or this is the result of taking medications that contain substances that violate the peristalsis of the esophagus.
Main reasons:
- hereditary abnormal disorders of the structure of the neuromuscular system of the esophagus
- stressful situations
- states of neurosis
- hysteria
- alcoholism
- age changes
There are a number of diseases leading to esophageal dyskinesia:
- esophageal diverticula
- esophagitis
- hiatal hernia
- tumor-like formations
- scleroderma (connective tissue damage)
- muscle dystrophy
- peptic ulcer
- chronic cholecystitis
- diabetes
- severe functional lesions of the nervous system
Classification and diagnosis:
All dyskinesias of the esophagus are subdivided into those associated with impaired peristalsis of the thoracic esophagus and associated with impaired activity of the esophageal sphincter. The first include hypermotor disorders of the thoracic motility (increased contractions of the esophageal muscles) and hypomotor disorders of the thoracic motility (weakened contractions of the esophageal muscles).
Hypermotor disturbances of the peristalsis of the thoracic esophagus include:
- segmental esophagospasm or "nutcracker esophagus" (when individual parts of the esophagus are involved)
- diffuse esophagospasm (widespread throughout the esophagus)
- nonspecific movement disorders)
Hypermotor disorders are usually manifested in increased peristalsis and tone of the esophagus and are characterized by a certain set of symptoms (dysphagia, "Lump in the throat", chest pain). These violations make themselves felt both during the period of swallowing and outside this period. Hypomotor disturbances of thoracic motility can cause the development of reflux esophagitis, and also be accompanied by cardia insufficiency.
Sphincter dysfunctions include:
- dysfunction of the upper esophageal sphincter
- dysfunction of the lower esophageal sphincter
Dysfunction of the upper esophageal sphincter manifests itself in difficulty swallowing and is associated with a weakening of sphincter pressure and esophageal reflux.
Lower esophageal sphincter dysfunction includes:
- gastroesophageal reflux disease (cardiac insufficiency)
- achalasia of the cardia (cardiospasm)
- segmental esophagospasm (the so-called "nutcracker esophagus") - this variant of the development of dyskinesia is caused by spasm observed in certain parts of the esophagus.
Symptoms:
- dysphagia (even with semi-liquid food)
- mild pain in the middle and lower third of the sternum (without irradiation to other organs). The pains gradually develop and also gradually subside.
- spasms of individual parts of the esophagus revealed by fluoroscopy and esophagotokimography
Diffuse esophagospasm is characterized by the following symptoms:
- palpable pain in the sternum and in the epigastric region, caused by abnormal contractions of the thoracic esophagus, extending upward at high speed and radiating to the frontal chest, shoulder or even the lower jaw. Pain may or may not be associated with swallowing. Duration of pain from 30 minutes to several hours
- dysphagia (not systematic)
- belching
- spontaneous spasm of the esophageal walls revealed by fluoroscopy and esophagotokymography
Movement disorders of a non-specific nature have the following symptoms:
- dysphagia (rare)
- pain in the upper sternum and in the middle third of the sternum (variable in nature and of varying degrees of intensity, usually with meals)
Diagnosis of hypermotor dyskinesia of the esophagus is complicated by the need to differentiate with angina pectoris, achalasia of the cardia, esophageal cancer and gastroesophageal reflux disease.
Hypomotor disturbances of the peristalsis of the thoracic esophagus are determined by the following signs:
- dysphagia
- feeling of heaviness in the stomach
- belching
- esophagitis
- ingestion of food from the esophagus or stomach into the respiratory tract
Treatment:
First of all, concomitant diseases are detected, then they are differentiated with angina pectoris, achalasia of the cardia, gastroesophageal reflux disease, and esophageal cancer.
Hardware studies of the esophagus are performed. After confirming the diagnosis, drug treatment is prescribed. If dyskinesia is one of the symptoms of the underlying disease, then its treatment is reduced to treating the disease that caused the dyskinesia.
It is recommended to avoid body positions that increase reflux, reduce psycho-emotional and physical activity, and exclude alcohol. It is necessary to sleep on a raised headboard. Eliminate the intake of excessively cold or excessively hot food, spicy foods, spices, carbonated drinks, juices of sour fruits and vegetables, coarse fiber. The daily meal is split 4-6 times. In this case, the food should have a mushy consistency.

Read

Read