General microbiology - viruses, bacteria, fungi >>>> Opportunistic infection - what is it?
Opportunistic infection - what is it?
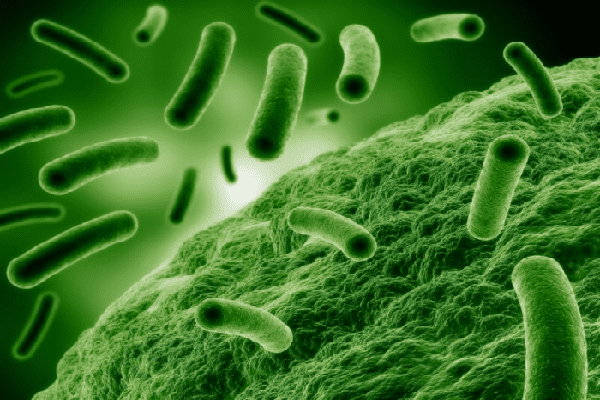
A person is able to get along with a variety of microorganisms, which, under certain circumstances (of a controlled number), are quite harmless, and can even serve a good, existing at the expense of the waste of useful microflora - by disposing of this waste. These microorganisms, called opportunistic microflora, are actually highly virulent, but in conditions of limited numbers they cannot destroy healthy cells or produce enough toxins to cause significant harm to the human body.
Conditionally - a pathogenic microorganism becomes an opportunist when it manages to uncontrollably increase the number and accordingly change the concentration of toxins or increase the damage to human cellular structures.
The number of conditional pathogens is controlled by the human immune system, which, with well-functioning immune mechanisms, quite copes with this task. But when the immune system itself is malfunctioning, it opens the door to opportunistic infection - the colonization of the body with pathogens.
Which microorganism can become an opportunist? These are viruses, bacteria, fungi, prions, protozoa. For example, staphylococcus aureus, with which a person gets along quietly in the absence of violations of the integrity of the skin and mucous membranes, can become an opportunist, just overcoming these barriers, and at the moment when a person's immunity is weakened, increase its number and spread through all tissues of the body in a very short period time.
Opportunistic infections, as a rule, acquire a chronic course of the disease and have latent course forms. This happens due to the impossibility of changing the state of the immune response to an antigen (an opportunistic microorganism) with incorrectly flowing protective biochemical reactions - immune reactions. In other words, the immune system cannot accurately determine the presence of an antigen, does not produce specific antibodies to its presence, and tests do not show the presence of antibodies to microorganisms - opportunists, which leads to the impossibility of developing mechanisms for treating an infectious disease - an opportunistic disease.
The ways of spreading opportunistic infection are diverse: contact, blood contact, lymphogenous, fecal - oral, aerogenic, transmissible, sexual, transplacental. Any local focus of infection in the body can provoke an opportunistic infection with weak immunity or improper treatment tactics.
Immune system inefficiencies resulting from opportunistic infections can be attributed to a number of factors:
- Weakening of immunity in connection with the intake of immunosuppressants (for example, cytostatics for the treatment of tumors, immunosuppressants for autoimmune diseases or organ transplants);
- Congenital or acquired immunodeficiency;
- Long-term uncontrolled antibiotic therapy, reducing the number of beneficial microflora, which entails the absence of a deterrent for the reproduction of opportunistic microorganisms.
An example of opportunistic microorganisms can be: herpes simplex virus, Escherichia coli, staphylococci, streptococci, cytomegalovirus, Klebsiella, Toxoplasma, Candida fungi and many more microorganisms.
Today, ELISA (enzyme-linked immunosorbent assay) and PCR (polymerase chain reaction - identification of RNA and DNA of microorganisms) allow to identify chronic opportunistic infection. These are the most effective methods of biochemical diagnostics and recognition of harmful microorganisms - opportunists.

Read

Read