Cardiovascular system >>>> Left ventricular failure
Left ventricular failure.

The activity of the heart is determined by the contractile function of the myocardium; heart rate; the possibilities of stretching the myocardial fiber (which determines the strength of myocardial contractions); the force developed by the contracting muscle of the myocardium. With the development of heart failure, the contractile function of the myocardium is the first to suffer, in the case of the development of left ventricular failure the contractile function of the myocardial muscle of the left ventricle suffers. The left ventricle cannot cope with the release of the entire volume of blood entering it, causing the pulmonary vessels to overflow with blood. The result of this phenomenon is increased blood pressure in the pulmonary veins and capillaries, gas exchange is disrupted. Blood plasma leaves the walls of the capillaries and enters the alveoli, filling them with liquid contents, and the gas in the alveoli, mixing with the liquid, forms a foam. This is how alveolar edema appears, followed by pulmonary edema.
The causes of left ventricular failure lie in a number of diseases that load the left side of the heart muscle:
- coronary heart disease (including heart rhythm disturbances ),
- cardiomyopathy,
- myocardial infarction,
- postinfarction cardiosclerosis,
- diffuse myocarditis,
- cardiogenic pulmonary edema,
- hypertonic disease,
- symptomatic arterial hypertension (for example, with impaired renal function, with endocrine diseases, with diseases of the nervous system, drug hypertension, hemodynamic hypertension),
- mitral stenosis,
- excessive filling of the bloodstream with fluids (with the introduction of solutions intravenously),
- obstruction of the lumen of the pulmonary vein (for example, with thromboembolism),
- uremia.
Signs of left ventricular failure develop gradually:
- in the early stages, the volume of cardiac output does not decrease due to an increase in heart rate,
- shortness of breath increases during physical exertion,
- tachycardia develops,
- there is a cough,
- with hardware examination noticeable expansion of the size of the heart to the left,
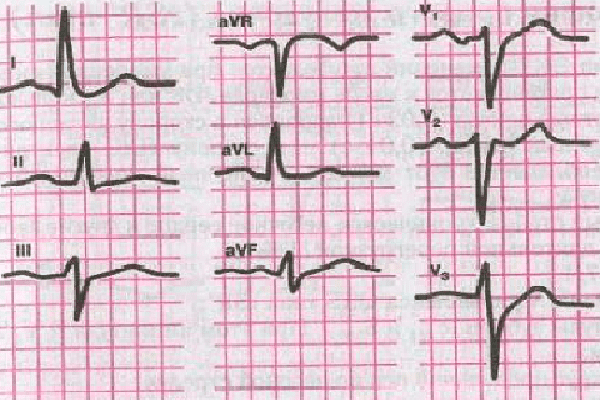
- a cardiogram shows the horizontal electrical position of the heart, signs of left ventricular overload and hypertrophy,
- the symptoms of cardiac asthma gradually increase ,
- there are symptoms of respiratory failure .
Treatment of left ventricular failure.
Treatment for left ventricular failure differs depending on whether the process is in acute or chronic phase.
The chronic form of left ventricular failure requires:
- stable emotional state,
- unloading the pulmonary circulation by taking diuretic drugs (synthetic and herbal diuretics ),
- treating hypertension by taking antihypertensive drugs (lowering blood pressure),
- treatment of diseases that provoked left ventricular failure.
Acute left ventricular failure requires immediate measures to prevent pulmonary edema and is associated with the relief of symptoms of cardiac asthma preceding pulmonary edema:
- They reduce the intensity of metabolic processes for better tolerance of a lack of oxygen (morphine - depressing respiration and lowers pressure (there are contraindications); droperidol - has a sedative effect; for those suffering from hypotension, sodium oxybutyrate is recommended - it has a sedative effect and normalizes blood pressure).
- Decrease in venous return of blood to the heart (dilatation of the coronary arteries (nitroglycerin), in severe edema - sodium nitroprusside, the application of tourniquets (see article "Cardiac asthma"), instead of a tourniquet, you can use a cuff from a pressure monitor (two cuffs are needed)).
- Fast-acting diuretics make it possible to reduce the load on the pulmonary circulation (furosemide, uregit) and are administered intravenously.
- In the absence of the above-described medicines, gangioblockers are used (intravenously), which reduce the pressure in the pulmonary and systemic circulation (Pentamin, Arfonad). The use of ganglion blockers should be monitored by frequent blood pressure measurements (every 3 minutes) on the free arm. With arterial hypotension, ganglion blockers are contraindicated.
- Oxygen inhalation (oxygen therapy) with a catheter or mask.
- Increasing the contractility of the myocardium against the background of arterial hypertension by taking dopmine or dobutrex.

Read

Read